Putting Tissue to the Test: 3D Organ Bioprinting
By Kevin Ritchart
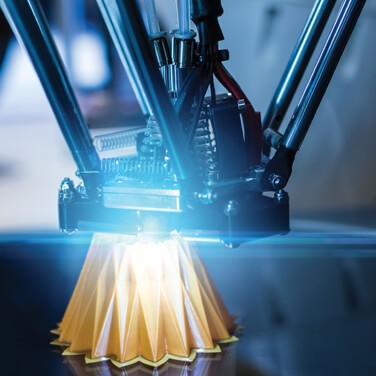
A recent breakthrough has brought bioengineers even closer to creating replacement organs using 3D printing.
Scientists have discovered a new technique for bioprinting tissues that includes structures that function like the body’s complicated natural vascular networks. Their research was published in an issue of Science earlier this year.
A team of scientists worked with a Massachusetts design firm called Nervous System to create a hydrogel model of a lung-like air sac that has airways to deliver oxygen to the blood vessels that surround it.
“One of the biggest road blocks to generating functional tissue replacements has been our inability to print the complex vasculature that can supply nutrients to densely populated tissues,” said Jordan Miller, assistant professor of bioengineering at Rice’s Brown School of Engineering.
Supply and Demand
The primary impetus for bioprinting healthy, functional organs is the overwhelming demand for organ transplants. In the U.S. alone, more than 100,000 people are on transplant waiting lists. Those who are fortunate enough to receive a transplant must still fight with immuno-suppressing drugs to keep their bodies from rejecting the transplants.
Organ bioprinting, once perfected, may be able to solve both problems. Organ replacements can be produced based on need, reducing the long waiting lists for healthy and compatible matches. And the replacement organs could be printed using the patient’s own cells, which would eliminate the potential for rejection.
To tackle this challenge, the research team created a new, open-source bioprinting technology called the “stereolithographing apparatus for tissue engineering” or SLATE for short. The system employs an additive manufacturing technique to construct soft hydrogels one layer at a time.
"We are only at the beginning of our exploration of the architectures found in the human body."
Let There Be Light
The layers are printed using a liquid pre-hydrogel solution that transforms to a solid when it’s exposed to blue light. A digital light-processing projector shines light from below at 2D slices of the structure. When each layer is solidified, an arm raises the growing (and now 3D) gel just enough for the next liquid layer to be exposed to the light.
A key component of the process is the use of food dyes that can absorb the blue light. This allows extremely thin layers to be solidified and makes the SLATE system ideal for quickly producing soft, water-based, and biocompatible gels that have complex internal structures.
Go with the Flow
Tests of a lung structure that was created using this process produced tissues that are strong enough to avoid bursting during blood flow and the pulsatile and rhythmic intake and outflow of air that mimics human respiration.
Red blood cells could also take up oxygen as it flowed through the vessels surrounding the 3D printed “breathing” air sac. This movement of oxygen is analogous to the gas exchange that occurs in the lungs’ alveolar air sacs.
The teams are also experimenting with implanting liver cell-containing bioprinted constructs into mice. These “tissues” had separate compartments for blood vessels and liver cells and were implanted in mice with chronic liver injuries. Tests showed that the liver cells survived the implantation.
Access for All
Because this groundbreaking research was facilitated and enabled by open-source projects, Miller and his team are supporting the further development of this potentially life-saving technology. He and the team have made all of the SLATE-related source data from their experiments and the 3D printable files freely available to other bioengineers.
Miller’s lab is already using the new design and bioprinting techniques to explore even more complex structures. “We are only at the beginning of our exploration of the architectures found in the human body,” he said. “We still have so much more to learn.”