Simplifying Immune Oncology Research
Novel 3D Tumor Model Streamlines High-Throughput Immunotherapy Testing

Immunotherapy has become a topic of increased interest for scientists studying cancer. By using a patient’s own immune cells to attack cancer cells, immunotherapy treatments have shown positive results, including total cancer remission in some cases. But immunotherapy is not a one-size-fits-all approach; treatment strategy and efficacy can vary by patient and cancer type.
To more carefully study immunotherapy as a cancer treatment, scientists need efficient, in vitro screening models to examine targeted therapy options. This type of research has historically been conducted with cell culture models that allow for the study of immune cell migration, which can be easily adapted for high-throughput screening. However, these models typically utilize two-dimensional (2D) cell culture monolayers that do not accurately reflect a tumor’s complexity in the human body. The current growing trend is to use more in vivo-like three-dimensional (3D) models.
To incorporate the immune cell component, these 3D models require the direct addition of immune cells to 3D spheroids. However, this may not be an accurate reflection of how immune cells migrate toward and further invade tumors in vitro. According to Hannah Gitschier, Corning Life Sciences Applications Lab Manager in Kennebunk, Maine, “With immunotherapy, it is imperative that researchers have solid models to best recapitulate the in vivo microenvironment and interactions between the engineered immune cells and patient tumor samples. These models must be easy to use and transferrable to a high-throughput screening environment, enabling rapid screening of conditions to best predict clinical outcomes.”
Traditionally, 2D assays were the method of choice given the high proliferation rate of cells in 2D culture, as well as the reproducibility of assays. However, with emerging technologies and the development of novel lab consumables, 3D assays are becoming easier to adapt and more relevant for researchers' end goals.
Creating a Better Way
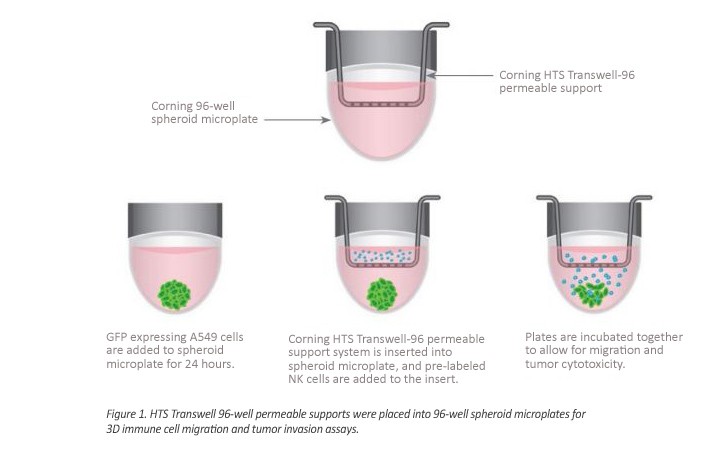
Hilary Sherman, a Corning Applications Scientist, created a 3D culture model to observe immune cell and tumor cell interactions; she combined the Corning 96-well spheroid microplate with the high-throughput screening (HTS) Transwell-96 tissue culture system. Coated with Corning’s unique Ultra-Low Attachment surface, the spheroid microplate allows for highly reproducible, single multicellular tumor spheroids to form in each well.
The HTS Transwell permeable support systems are commonly used in migration and invasion studies, with a flat-bottom receiver plate for monolayer culture. This novel combination of both products allows researchers to observe changes to tumor behavior — by adding immune cells to the Transwell insert, the rates of migration through the membrane and toward the tumor spheroids in the receiver plate can be observed. Combining the technologies allows one to study how these two cell types interact in a more in vivo-like environment.
Sherman placed the spheroid microplate under the HTS Transwell insert plate instead of using the flat-bottom Transwell receiver plate. This enabled her to observe tumor cell activity in a 3D system while also facilitating migration of immune cells toward the tumor cell model. This technique supports the investigation of immune cell homing, tumor toxicity, and tumor immune evasion in an easy-to-use, reproducible, 3D high-throughput assay.
Study Methods
Cells from a cancerous lung tissue cell line (A549 cells) were seeded into 96-well spheroid microplates to form the tumor spheroid models. The following day, Sherman placed the HTS Transwell 96-well permeable supports in the spheroid microplates. To assess immune cell homing and migration, natural killer (NK) cells were added into the inserts and were allowed to migrate for 24 hours. (See Figure 1.)
Implications on Future Research
A successful model allows for the immune cells to reach the tumor cells of interest in order to effectively study the body’s response to targeted immunotherapy. Sherman’s novel research model confirmed the NK cells in this study were not only able to reach the target tumor cells but could also infiltrate the 3D spheroid structure and lead to the desired cytotoxic outcome.
This creates a more streamlined model to observe all necessary components of this immunotherapy research in a single, high-throughput, reproducible in vivo-like format.
“This model allows researchers to study immune system-tumor interactions in a more comprehensive way that also has the benefit of being high-throughput and easy to use. The system can also be used to study other immune and cancer cells as well as the ability to form more complex models by adding endothelial or glial cells to the Transwell membrane to create more advanced blood brain barrier models,” says Gitschier.